Bere 5/2025 #16
Continued…
I’m about to drift off to sleep, laying there wet and evaporating in the fan when I get a call. It’s difficult to hear what the nurse is saying as there is a lot of background noise on his end. I think he says someone can’t pee and has a catheter in and is in a lot of pain.
I had seen a man brought into the recovery area carried by his family members because he wasn’t peeing with a catheter in. One of the other docs was out there and I was trying to get to my next surgery so I walked away to my surgery figuring they would figure out what was going on. So as I get my self together and grab my bag of stuff (water, stethoscope, headlamp, butterfly ultrasound, kind bars, batteries for headlamp) and head to the hospital, I wonder if it is for that same man. Wondering if the foley balloon was blown up below the prostate, breaking the urethra and causing a stricture in the future…
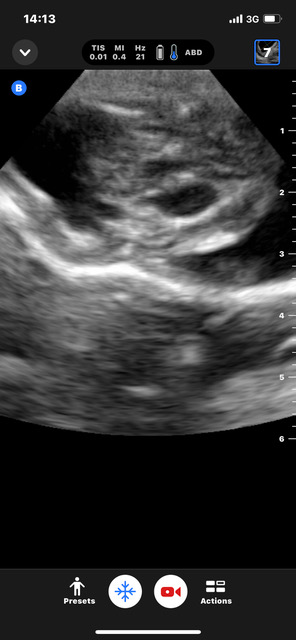
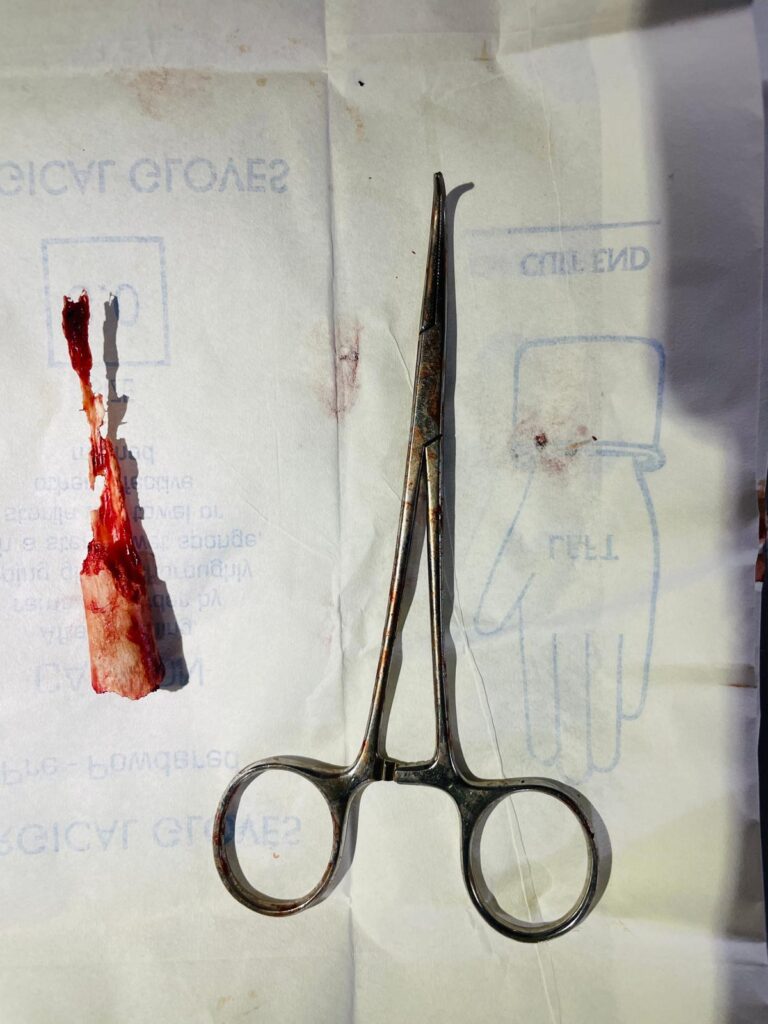
I walk through the ER and adult wards looking for the patient. Not there. So I go to the surgical ward and he’s there. It is the same old man. Three women are fanning him with handheld fans- a sign that he is in distress. They fan when someone is after surgery and when they are really hurting or agitated. The man is grunting and I ask him what’s going on. He tells the nurse that he can’t pee and his abdomen hurts. There is only about 5cc of urine in the tubing not making it to the foley bag. And so I suspect it is misplaced in the urethra so I feel for a distended bladder. I don’t feel one. Hmmm. Same foley of earlier today? Yes. Same bag as earlier when you were in the OR? Yes. Is he not making urine?? I feel around his abdomen and he cries out in pain. Peritonitis. I get my Butterfly ultrasound and look for his bladder. I can barely see it for all the other fluid in his abdomen. So I attribute this to a leak from his intestine or stomach causing the peritonitis and lack of urine output. I see his CBC was ordered today by another doctor in clinic and they don’t have the paperwork but I can see on the computer his WBC is 20 and Hb- 17.1 So he’s very dehydrated, has peritonitis, not making urine. He hasn’t had a set of vitals, and I know I need to take him to the OR. So I call in Phillipe and try to get the medical student Caleb on the phone to help me. Caleb doesn’t pick up with multiple calls. So I walk to his house, shine my light in his screen window at him and say his name louder and louder till he awakens. Then I head back to open the OR and get the patient over there. It is now midnight. The surgery ward nurses put in another IV – good job, without my thinking of asking. I ask them to bring the patient to the OR and go and start unlocking the OR and turning on lights and machines. They wheel him in on a stretcher. While I wait for Phillipe I hook him up the the anesthesia monitor and start the BP cuff. HR- 120 BP 70/30. I start pouring in the fluids. He’s very dehydrated, likely in shock. Phillipe and Caleb arrive and after a few liters of fluid his BP and HR are better. He’s also looking a little better though very sick. I wish I had an ICU for him. I open the OR pack, select my suture, scalpel blade, cloth sheath for the cautery, pack of the reused suction tubing, our sterile gloves, gauze, and get everything ready. I prep his abdomen with betadine then go scrub. I scrub with the brown bar of soap then go back in to the OR, dry my hands and put on my sterile cloth gown and gloves. I gown and glove Caleb. We pray for Gods guidance and keeping this man alive during and after the operation and we start. I cut through the skin and very small fat and into the fascia and abdomen. As soon as I enter the intestinal contents start flowing out. We suck all of it we can but it still pours all over getting our gowns (and us) wet. I start in the middle looking for a hole and then extend my incision top to bottom looking for it. I see a dark patch in the terminal ileum, but see no hole. AFter looking at all the bowel and stomach again, I come back to the dark patch. I now squeeze intestinal contents towards the area and sure enough, I see a small pinhole leaking. So this has been leaking a while to get all this into his abdomen! Phillipe says START CHEST COMPRESSIONS! What? He hasn’t told me the pressure has been real low and up and down the whole surgery thus far. I start compressions. I ask him questions. The patients BP has been between 80 and 40 systolic and now not registering. I reach in the abdomen and feel the heart still beating. He gives a slug of ephedrine into the side of the IV container and its running wide open. The SBP picks up to 40 then 60. I need to be done this operation as soon as possible. I wish I had staplers but I don’t. So I take out that section of intestine with clamps on either end. Phillipe is giving two units of blood. I think the patient may not need blood, but he does need a blood pressure and he tells me he’s given many more liters fo crystalloid already. I choose to oversew the distal end in the sake of time and bring out the other end as an ileostomy. I wash out the belly with multiple liters of fluid that goes all over. I close the fascia and the patient is still alive- barely. I put the stitches to form the ostomy and leave the skin open in the sake of time. Phillipe extubates him after about 30 min and he goes to the “recovery” room. Meaning he gets out to a room where there is a monitor and the family can come and see him. The women start fanning and everyone just stares at him wondering if he is alive and looking for breathing. I tell the family what we did and show them the piece of intestine we took out. I suspect it’s a typhoid perforation. It’s 4:30 and Phillipe says he’ll start with the patient. I head back to sleep. I get 3 hours before my alarm goes off to start today…
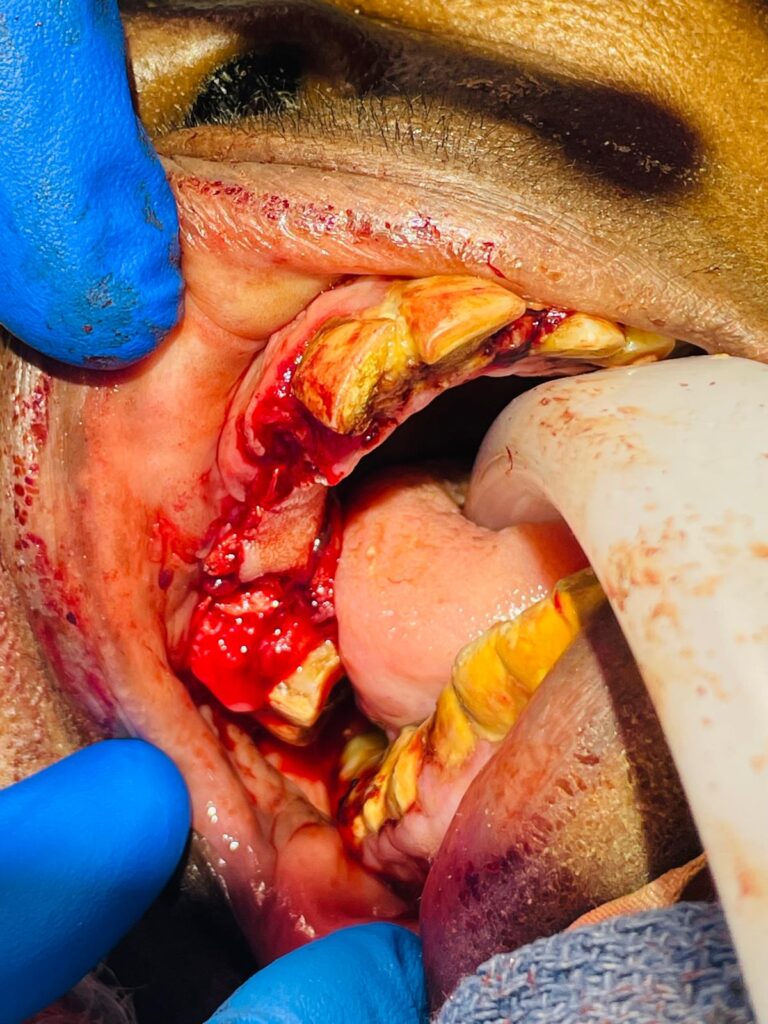
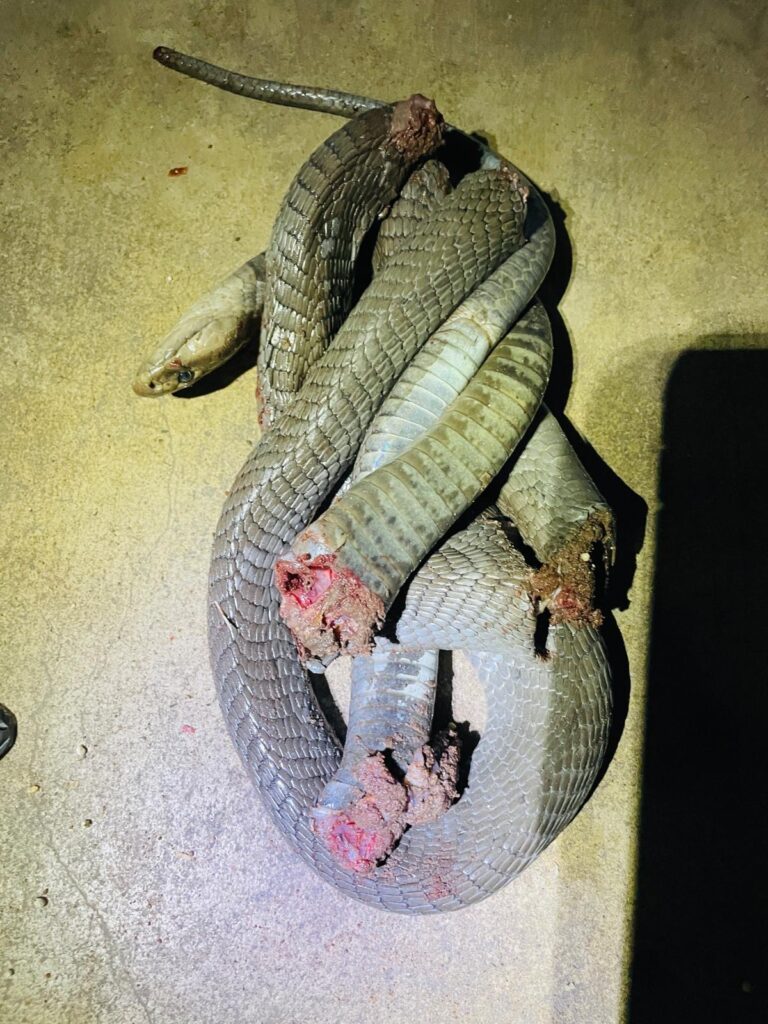
I am deep asleep but know I must get up. There are 6-8 patients scheduled for surgery today and no way to get through them if Im not operating. I go in and find that David is doing anesthesia and Phillipe hasn’t come in. Drs. Andrew and Steven are doing a thyroid that is huge soon and so I head to do rounds where I find my patient still alive, women standing at bedside fanning and the patient minimally responding to questions. Again I wish I had an ICU with ICU nurses, monitoring and meds…. Wish for so many things. My cow horn goring guy wants to go home. As I think another operation will just delay a day or two the inevitable, I agree and discharge him home. I pray with him asking for Gods miraculous healing and encourage him to keep his trust in God till the end.
I go to clinic and am there till my last patient is about 3PM. Phillipe isn’t coming in today so only on room can operate. The OB/GYN is getting ready to do a hysterectomy (take a uterus out) on a woman with a huge uterine fibroid. Her uterus is well above the umbilicus. I wait till her patient is intubated to make sure it goes well then I head to say goodbye to the other missionaries. Missionaries I rarely see because they are spouses of the doctors or others that don’t work in the hospital and I don’t run into often.
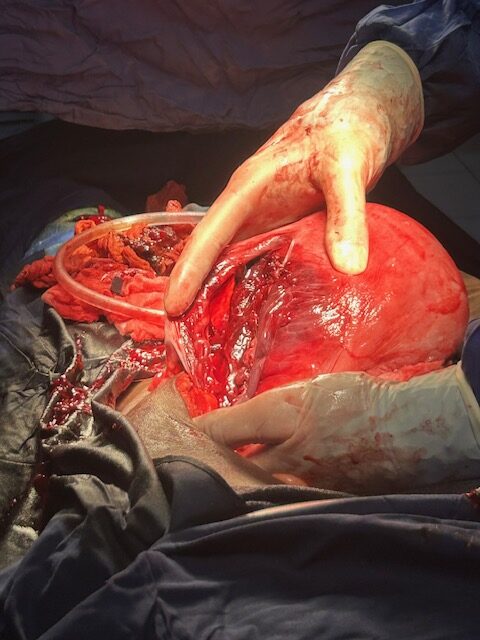
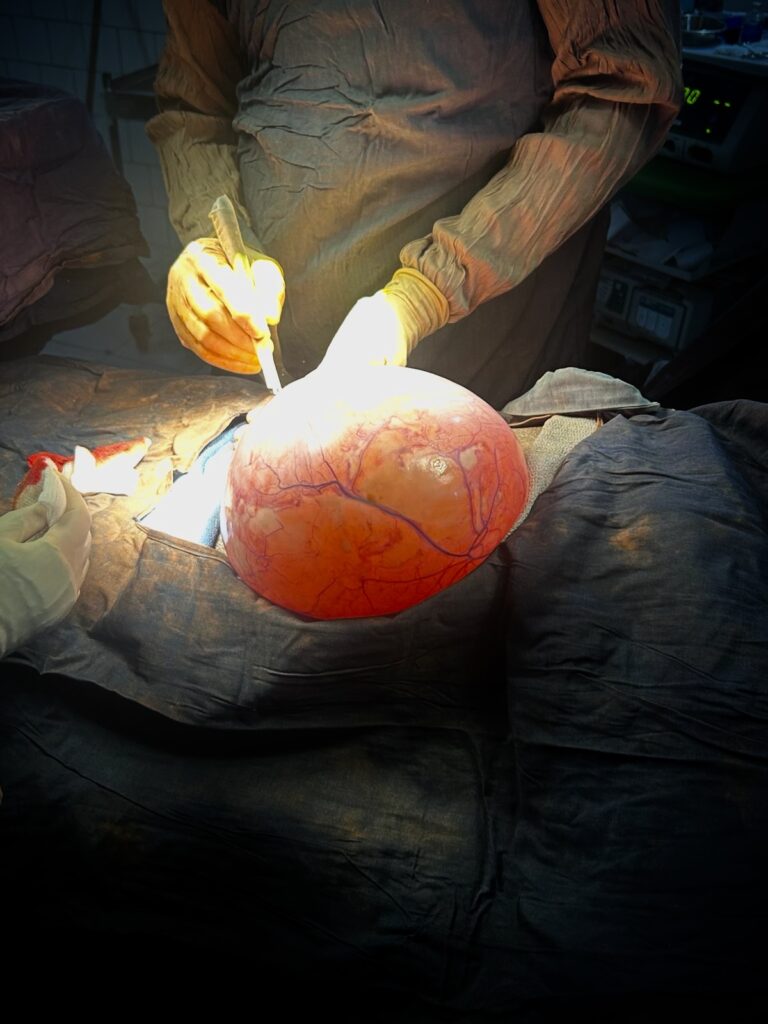
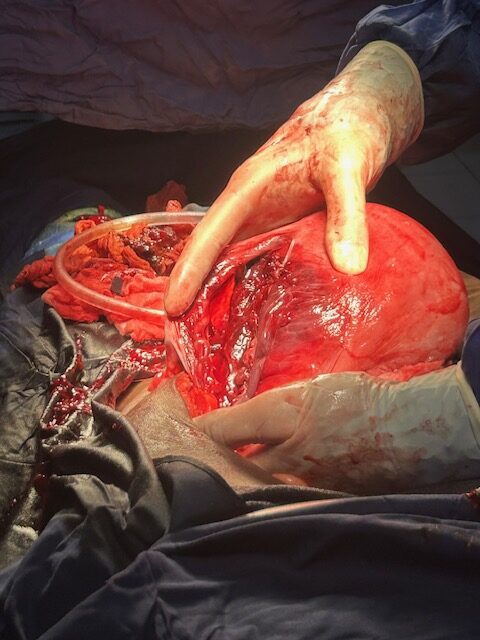
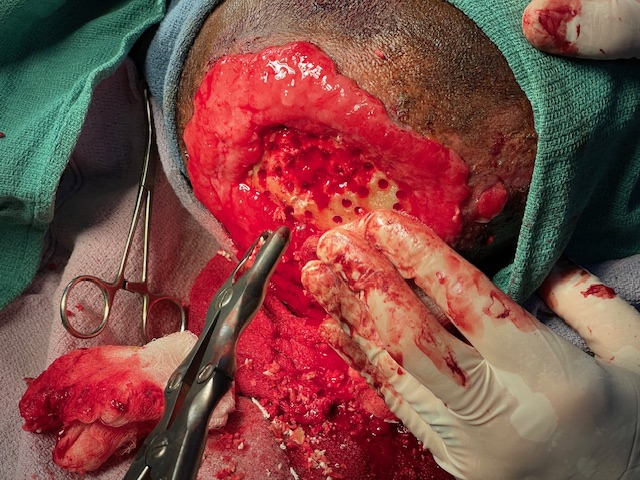
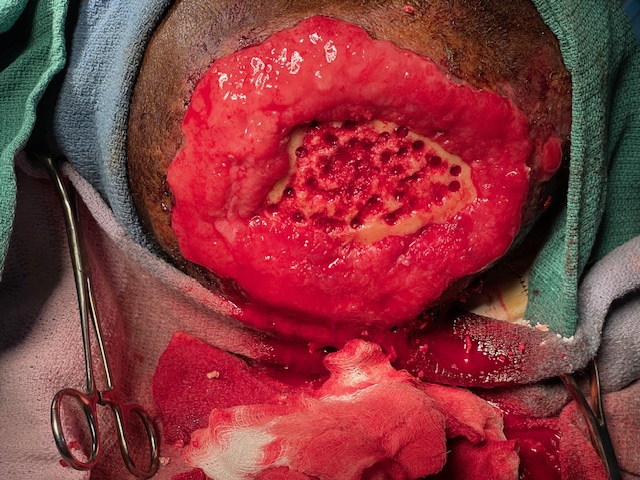
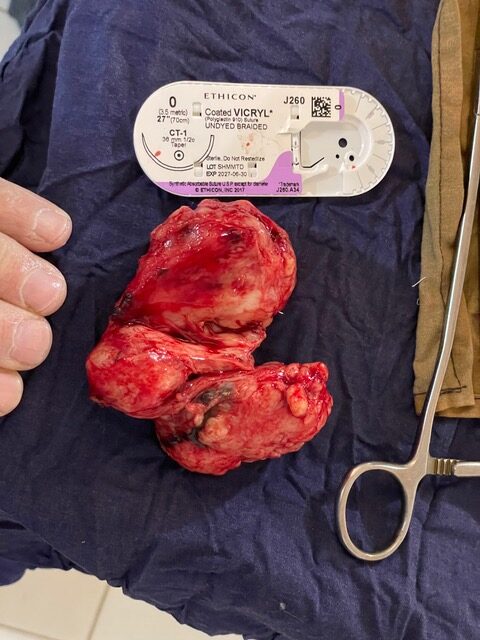
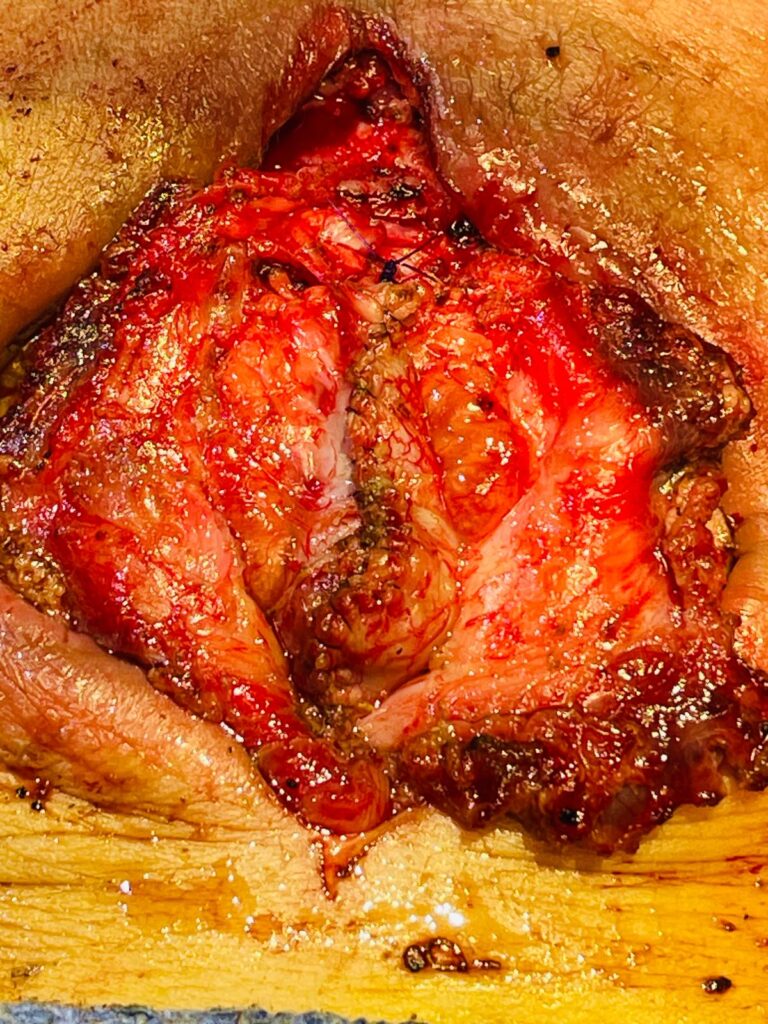
About 6PM I get a call can I come help the OB/GYN in the OR. I hear there is bleeding and it’s a real tough case. It’s her first time in Bere and I wonder if it’s real hard or she she’s not used to the lack of equipment… I glance in the room before scrubbing. There is blood all over the abdomen and down the sides of drapes onto the floor. How could I doubt her! It looks bad. The patient is getting blood and a low BP but not life threatening low. I choose to forgo the plastic apron, because of it’s heat, and dawn the cloth gown. I later regret this decision. I take the place of the medical student and he becomes the scrub tech handing instruments to us. Which in this surgery is very helpful!! I pull hard on the uterus and it doesn’t budge. It is the size of at least a football, nearly a basketball. I pull to the side trying to expose for her and we get 1cm between it and the pelvic sidewall. OOHHH! This is terrible. No wonder she needed help. This is the worst I’ve seen for lack of visualization. We do our clamps, cut tie, down the sides further. ¼ in by ¼ in. Very small increments. We hug the uterus hoping we are not coming close to the ureters or iliac vessels. Usually as you go down the uterus becomes more and more mobile and comes up into the incision more and more exposing the next area to take. This one doesn’t move. We march down the sides with very little space to see anything, praying we don’t get into deep bleeding that would kill her before we could control it. As I work I soon realize the lack of the apron is making the patient blood soak through my gown, scrubs and underwear. I hate that feeling. Knowing I’m wet from someone else’s fluids… I mention maybe if wee took the posterior peritoneum, if we can get there, maybe we would get a little upwards movement. So she divides posterior and we are into the uterus next to the fibroid. It starts pealing out of the uterus. In 20 seconds we have the top of the uterus off with it’s huge fibroid and now we can see. We start controlling the bleeding and she packs some surgical and other hemostatic agents she brought into he area we just tore the fibroid out of. Now we start looking for the ureters. The left we don’t see and the right we find very distended and know it’s tied off. So we start taking down the ties, which causes more bleeding and eventually get off the tie that is on the ureter. We realize we have tied, cut and divided the ureter. This is terrible an neither of us have done this before nor encountered it before. But we have both read what is to be done in this situation. We need to either repair the two ends back together or implant the end we found into the bladder. Her bladder is large and easily reaches this area so we plan on that. We cut up the ureter a short distance to (spatulate) or make the opening larger so that our anastomosis will be larger and less likely to stricture with healing. Then using PDS we suture the ureter to the bladder. As we close we take a ureteral stent and put it through the abdominal wall, into the lower bladder, then up through our area of anastomosis. This will help it stay open while it heals. We are both spent. The patient has stabilized and our visualization is tough with the intestines pushing into the area. We search for the other one unsuccessfully and check that there is some urine in the foley bag so we decide to close. It’s about 8PM. I have handed my call phone off to Dr. Stephen so I know I won’t get called tonight. But I need to eat supper and pack. I leave at 5 AM on a Moto for Kelo to catch the first bus to Ndjamena. Dr. Leslie and Caleb, med student, start closing and I head out for supper at Dr. Andrew and Dr. Meghans house. Instead I head to my room for a shower, because I look like I had a circumcision in the village. (They use the pull the foreskin and cut, technique in the village). I have about a 2 foot circle of blood coving from my lower chest to thighs. Yuck! As expected, in the shower that same area has blood on my skin.
At supper, Dr. Leslie calls, there’s not more urine in the “recovery” room and she thinks we need to look again at the other side. She has flushed the foley and there is no blood clot obstructing it. We all decide it can wait till morning and I head back to my room to pack. It get done about midnight and sleep deeply till my alarm awake me at 4:30. After I’m dressed I take my bags out, see Rebecca is waiting to say good by, and my luggage is strapped to the back of the Moto and I and the driver load up and we are off for the 2 hour ride to Kelo as the sun comes up.
I thank you each for your prayers and for your interest in the mission work God has been giving me over these many years. I pray for His continued Guidance in my life on a daily basis.
If you want to support Bere Adventist Hospital this is a link you can use for financial support:
https://www.paypal.com/donate/?hosted_button_id=8JLSUCVBGG7Q8
If you want to volunteer your abilities, time, and talents and whatever God has given you knowledge of- contact me via phone or email. All different abilities are needed.
God bless you as you serve Him wherever He leads you!


























 then, surprise, it didn’t go flat again. We made it to Bere about 8:30PM. So traveling from my house Tuesday afternoon I arrive in Bere Friday night. Long trip. I ate supper at a missionaries house and we talked a while and I finally got to bed about 1AM. I awoke at 5AM- jet lag…
then, surprise, it didn’t go flat again. We made it to Bere about 8:30PM. So traveling from my house Tuesday afternoon I arrive in Bere Friday night. Long trip. I ate supper at a missionaries house and we talked a while and I finally got to bed about 1AM. I awoke at 5AM- jet lag…